Recent Posts:
Revolutionizing Accessibility and Affordability in Prosthetics: A Life Care Planning Perspective
Neurodiversity Awareness
The Risks of Using Weight Loss Drugs Without a Prescription
j Revolutionizing Accessibility and Affordability in Prosthetics: A Life Care Planning Perspective
By Susan Wirt on April 24, 2025 | original article: Tech Briefs
The global reality for individuals with limb loss is stark—90% of amputees lack access to proper prosthetic care. This critical gap in healthcare and rehabilitation prompted LIMBER Prosthetics & Orthotics, Inc. to reimagine prosthetic development through innovative 3D printing technology. By creating structurally sound, one-piece prosthetic limbs, LIMBER is addressing the need for affordable, accessible solutions, significantly benefiting life care planning and rehabilitation case management.
LIMBER’s journey began at the University of California, San Diego, as a research initiative under the guidance of structural engineering professor Falko Kuester. The traditional process of crafting prosthetics, often described as a sculptural art form, involves labor-intensive hand-carving of residual limb models. This method is not only time-consuming and costly but also challenging to scale in underserved regions where prosthetists are scarce.
Recognizing the potential for improvement, Kuester collaborated with Ph.D. student Luca De Vivo Nicoloso. Together with Joshua Pelz, a fellow researcher, and Herb Barrack, a certified prosthetist with over three decades of experience, they founded LIMBER to modernize and streamline prosthetic fabrication.
LIMBER’s approach integrates advanced technology with personalized care, ensuring a seamless and efficient experience for patients and care teams. The process begins with a 3D scan of the patient’s residual limb using an iPhone (model 10 or later). This scan provides an initial geometric model, which is then refined by certified prosthetists who incorporate manual measurements and clinical expertise. This personalized design ensures each prosthetic limb addresses the unique needs of the individual, enhancing comfort, function, and mobility.
The collected data is uploaded to the LIMBER cloud, where it is reviewed and finalized by skilled design technicians and prosthetists. The finalized design is sent to LIMBER’s 3D printing facilities, where the prosthetic is manufactured, post-processed, and shipped to the patient’s care provider for fitting. This streamlined workflow reduces production times significantly, with prosthetics delivered in as little as one to two days in the U.S. and within a week internationally.
LIMBER’s commitment to affordability and accessibility is reflected in its two-pronged business model. In developed countries, the company sells custom prosthetics at competitive prices, while subsidizing services in developing nations to offer discounted or free prosthetics. Collaborating with local institutions, such as rehabilitation centers and community organizations, LIMBER ensures the solutions are culturally relevant and effectively meet the needs of underserved populations. For instance, partnerships with organizations like Rotary Clubs in Mexico demonstrate the company’s dedication to sustainable, community-centered care.
To date, LIMBER has successfully delivered 15 custom-designed prosthetic limbs, achieving a remarkable first-fit success rate. Minor adjustments, such as alignment or socket fit modifications, were easily resolved by prosthetists using LIMBER’s thermoforming technology. This adaptability minimizes disruptions to patient care and exemplifies the company’s focus on practical, patient-friendly solutions
LIMBER’s technology holds immense promise for life care planning and rehabilitation case management, offering a cost-effective, scalable solution to prosthetic care. By reducing production costs and enabling faster delivery, LIMBER empowers case managers and healthcare providers to support patients with timely, high-quality prosthetics that improve their quality of life.
With plans to begin selling 3D-printed prosthetic limbs in the U.S. in early 2024, LIMBER is poised to transform the landscape of prosthetic care, bridging the gap between innovation and accessibility for patients worldwide.
j Neurodiversity Awareness
By Susan Wirt on December 2, 2024 | original article: Newswise
In today’s healthcare landscape, the concept of neurodiversity has become increasingly important, influencing how we approach long-term care and support for individuals with cognitive and developmental differences. A poignant reminder of this shift occurred during the Democratic National Convention, when vice-presidential candidate Tim Walz shared the stage with his son, Gus, who lives with a nonverbal learning disorder and ADHD. This heartfelt moment touched the nation and sparked critical conversations about how society can better support people with neurodivergent conditions.
The Walz family’s openness about Gus’s neurodiversity has been a source of inspiration for many, shining a light on the importance of personalized, compassionate care. Neurodivergent individuals—those with conditions such as autism, ADHD, or learning disorders—often require tailored care plans that address their unique needs while recognizing their strengths. This approach ensures that their support systems, whether medical, educational, or social, are designed to promote independence, improve quality of life, and foster inclusion.
Creating comprehensive, individualized care strategies is key to helping neurodivergent individuals thrive. By understanding each person’s specific challenges, healthcare professionals can collaborate with families, educators, and therapists to develop support systems that offer meaningful resources—from specialized therapies to assistive technologies and educational accommodations. These strategies go beyond addressing medical needs; they focus on building a foundation for long-term success and fulfillment.
Healthcare professionals play a crucial role in advocating for individuals with neurodivergent conditions, ensuring they receive the appropriate therapies, medical care, and services to meet their unique needs. Navigating healthcare systems, coordinating care across various disciplines, and connecting families with the right resources are all essential in helping individuals achieve their full potential. It’s about bridging gaps between medical care, social support, and education, allowing individuals and their families to feel empowered and supported.
The increased awareness of neurodiversity, highlighted by moments like the Walz family’s story, emphasizes the growing need for inclusive and personalized care. As these conversations move further into the mainstream, the healthcare community must continue to advocate for changes that support individuals with neurological differences.
By embracing neurodiversity and recognizing the value of personalized care, we are taking important steps toward a future where every individual, regardless of developmental or cognitive differences, has access to the opportunities and tools they need to succeed. This shift toward understanding and supporting neurodiversity is essential to ensuring that all individuals receive the compassionate, individualized care they deserve.
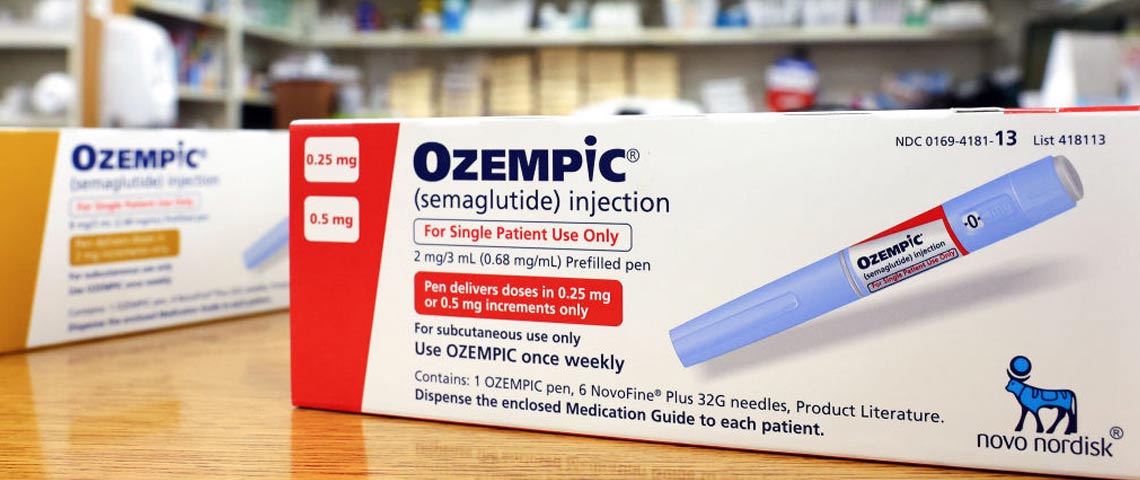
j The Risks of Using Weight Loss Drugs Without a Prescription
By Susan Wirt on November 20, 2024 | original article: Newswise
In recent years, injectable weight loss drugs like Ozempic and Wegovy have surged in popularity, offering hope for those struggling with weight management. Initially developed to treat Type 2 diabetes, these medications have also been found to curb appetite and slow digestion, leading to significant weight loss for some individuals. However, their increasing demand, coupled with high costs and limited availability, has driven some people to seek out alternative, often risky, solutions.
A national survey by The Ohio State University Wexner Medical Center revealed that 1 in 4 adults would consider using these medications without consulting a doctor. The motivations range from seeking more affordable options (18%) to facing difficulties accessing the drugs through pharmacies (6%). While the desire for quick results is understandable, bypassing professional medical guidance can pose serious health risks.
Dr. Shengyi Mao, an internal medicine physician at Ohio State, emphasizes the importance of consulting a healthcare provider before starting any medication for weight loss. “Every medication can have risks and side effects,” Dr. Mao notes, and only a trusted medical professional can evaluate an individual’s unique health needs and determine the safest path forward. This is especially true for medications like Ozempic and Wegovy, which, though effective for some, are not without potential complications.
One of the most pressing concerns is the rise of unregulated sources offering counterfeit or compounded versions of these drugs. The FDA has issued warnings about such alternatives, which may contain unapproved active ingredients, posing significant risks to those who use them. These unauthorized versions can lead to unpredictable side effects and undermine the safety that comes with proper medical oversight.
For individuals managing obesity, a complex and chronic condition, seeking out quick fixes can be tempting, but sustainable, long-term health requires a thoughtful, personalized approach. Weight loss should never follow a one-size-fits-all strategy, and decisions about treatment options must take into account each person’s medical history, health goals, and potential risks.
It’s important to remember that while medications like Ozempic and Wegovy can be valuable tools for some, they are just one part of a broader strategy for managing obesity. Addressing weight management holistically—through nutrition, physical activity, behavioral changes, and medical care—provides a safer, more effective path forward.
In this rapidly evolving landscape of weight loss solutions, the guidance of a healthcare provider is essential. A thoughtful, informed approach to care not only protects individuals from unnecessary risks but also sets the stage for long-term success and well-being.